Researchers may have unraveled the mechanism by which tumors resist anti-angiogenic agents (drugs that prevent tumor growth by impairing the formation of new blood vessels).
According to the study “Vessel co-option mediates resistance to anti-angiogenic therapy in liver metastases,” published in Nature Medicine, instead of generating new blood vessels, some tumors incorporate tumor cells in the vessel walls, a phenomenon known as vessel co-option, to obtain their blood supply.
Surgical removal of the primary tumor is a common procedure in cancer patients. But nearly half of patients with colon cancer who undergo surgery eventually recur and develop liver metastasis, which severely worsens their outcomes.
“Metastatic cancer is harder to treat than primary cancer — about 80 percent of patients diagnosed with colon cancer that metastasizes to the liver are inoperable,” Dr. Peter Metrakos, lead author of the study and director of the Multi-Organ Transplant Program and of hepatopancreatobiliary surgery at McGill University Health Centre in Canada, said in a press release.
“Chemotherapy has been able to prolong the lives of these patients, but it has not been able to provide a cure. If we can stop the metastasis, we have a better chance of curing patients,” he said.
The study was conducted by researchers from McGill and the Institute of Cancer Research in London.
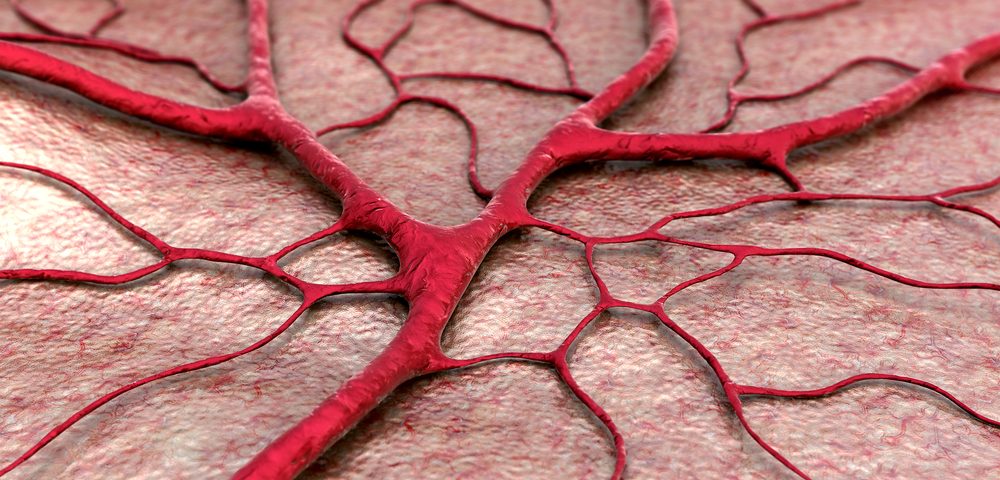
In an attempt to stop metastatic growth, investigators focused on angiogenesis, the formation of new blood vessels that support tumor growth by providing oxygen and nutrients.
In the last decade, researchers developed a number of anti-angiogenic therapies, including the anti-VEGF (vascular endothelial growth factor) Avastin (bevacizumab), which is now approved for the treatment of many different cancer types, including metastatic colorectal cancer in combination with chemotherapy.
But surprisingly, although these drugs could successfully slow cancer growth, the survival benefit of adding Avastin to chemotherapy was modest.
In recent studies, researchers found that metastasis can create blood vessels by the nonangiogenic mechanism of vessel co-option, a process where cancer cells incorporate pre-existing vessels instead of inducing the growth of new vessels.
Because anti-angiogenic drugs are not designed to target vessel co-option, the researchers hypothesized that this could be a significant mechanism of resistance to anti-angiogenic therapy in metastatic colorectal cancer.
Indeed, the team found that vessel co-option was the predominant mechanism of vascularization in nearly 40 percent of tumors. Also, metastases that used this technique were the most resistant to the anti-angiogenic therapy with Avastin, and patients were linked to lower overall survival rates when Avastin plus chemotherapy was used as treatment.
In addition, patients who progressed on Avastin often adopted vessel co-option as the prevalent mechanism of vascularization.
“We were treating all patients as if they were generating new blood vessels,” Metrakos said, “but our research has revealed that roughly 40-45 percent of tumors derive their blood supplies from new blood vessels, and another 40-45 percent derive their blood supplies by co-opting existing blood vessels of the liver to draw their blood, which explains why existing therapies that target new blood vessels are not working as well as predicted.”
“We thought tumors always generated the growth of new blood vessels but in some cases what they are doing is a little sneakier: The cancer cells surround the existing blood vessels of the liver to draw their blood supply,” he added. “We need to select our patients based on how their cancers obtain their blood supply and stratify them for the right treatment, essentially personalizing medicine.”
Preliminary work conducted by Metrako’s team suggests that this mechanism is not unique to metastatic colon cancer, and can also be happening in other tumors, such as lung, kidney, and brain cancer.
Now, more research is needed to develop new therapies that target vessel co-option and work in combination with anti-angiogenic therapies to prevent tumor growth.