A new study entitled “Accuracy of in vivo colorectal polyp discrimination by using dual-focus high-definition narrow-band imaging colonoscopy” shows that current imaging techniques used in colonoscopies are capable of assessing the benign or precancerous state of colorectal polyps, without the need for polyp extraction and pathological examination. The study was published in the December issue of the journal Gastrointestinal Endoscopy.
A new study entitled “Accuracy of in vivo colorectal polyp discrimination by using dual-focus high-definition narrow-band imaging colonoscopy” shows that current imaging techniques used in colonoscopies are capable of assessing the benign or precancerous state of colorectal polyps, without the need for polyp extraction and pathological examination. The study was published in the December issue of the journal Gastrointestinal Endoscopy.
Colorectal cancer is the third cause of death in both men and women cancer patients. In 2014, the American Cancer Society’s estimated 96,830 new cases of colon cancer and 40,000 new cases of rectal cancer occurring in the United States.
The guidelines for colorectal cancer prevention include screening procedures, by sigmoidoscopy or colonoscopy. In the latter, the clinician uses a flexible tube – colonoscope – that has an incorporated lens to screen both the rectum and the entire colon. Furthermore, it is equipped with a tiny set of “tweezers” to perform a tissue biopsy.
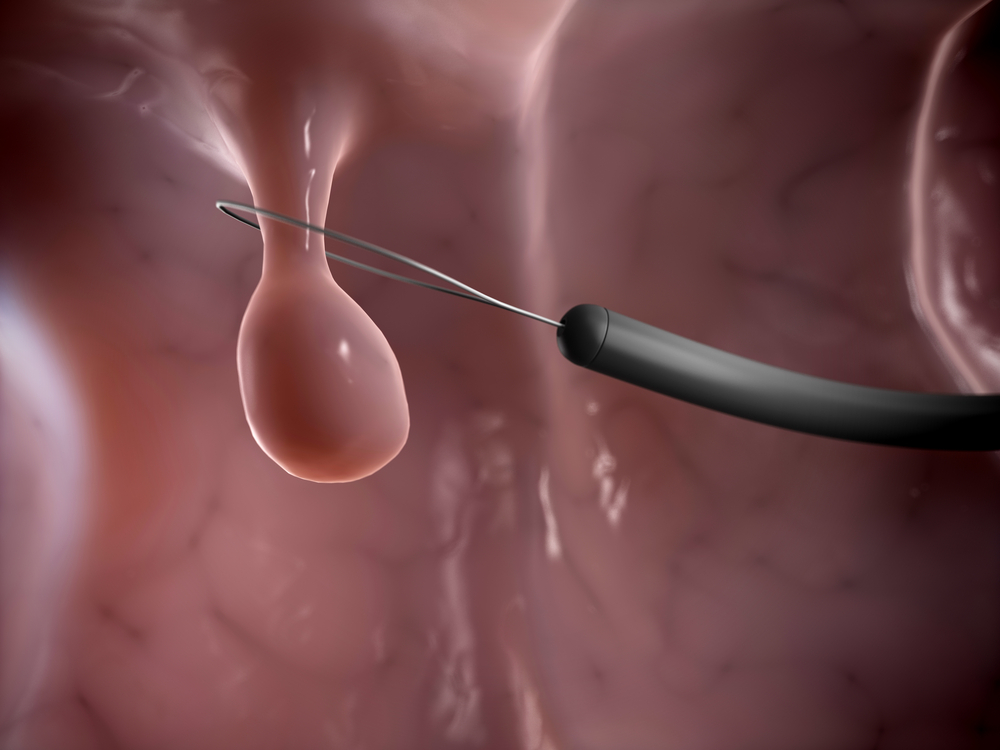
The majority of colorectal cancer begins with a polyp, an abnormal growth projecting from the lining intestinal membrane into the intestinal lumen. With age the formation of polyps is more common and, even though the majority are benign, some polyps –known as adenomas – are more likely to become cancerous. Thus, colonoscopy with polypectomy (the removal of a polyp) is indeed an efficient preventive measure and is associated with significant reduction in colorectal cancer deaths.
Current guidelines recommend the extraction of all visualised polyps during a screening procedure by colonoscopy for pathological examination. This, however, carries huge costs.
In this study, a team of researchers at the Mayo Clinic assessed whether new high-definition colonoscopes, that are equipped with a dual-focus imaging, can evaluate polyps at a precancerous or benign state without the necessity of removal and follow-up analysis.
As such, they screened 522 patients at an average risk of developing colorectal cancer and randomized patients to be submitted to a standard colonoscopy (with Olympus CF- H180 and Exera II 180 colonoscopes) or to dual-focus colonoscopy (the authors used the high-definition Exera II 180 colonoscope and the Exera III 190 colonoscope).
The team analyzed 927 polyps and compared the results obtained to an histological examination. They found that using both systems, standard and high-definition colonoscopy, is an efficient and reliable method to detect and distinguish between precancerous or benign polyps, with an accuracy of 96 or 97 percent, respectively. Additionally, physicians using both colonoscopes obtained an adenoma detection rate extremely elevated, with 50 percent (for the 180) and 52 percent (for the 190) detection. Of note, both systems are in agreement with the American Society for Gastrointestinal Endoscopy (ASGE) guidelines for optical diagnosis of colorectal polyps without the necessity of histologic examination.
Michael Wallace, M.D., MPH, gastroenterologist and leading author of the study noted in a press release, “A high adenoma detection rate is considered a good measure of a quality colonoscopy. Studies have shown that a rate of 33 percent — meaning that of 100 people who undergo a colonoscopy, adenomas are found in 33 percent — is excellent. Current national benchmarks recommend an adenoma detection rate of at least 20 percent. We found substantially more adenomas. The more adenoma polyps that are detected, the lower the risk is of getting colon cancer. So this study shows that it is possible to use an optical scope to perform a highly accurate colonoscopy and bypass the pathology laboratory, reducing cost. Another advantage is that we can tell the patient immediately after the procedure what we found and when the next examination should be done, as opposed to waiting one to two days for a pathology result.”