Though immune checkpoint inhibitors are deemed as especially promising in a number of cancers, the therapy often fails to exert an effect in more lethal cancers. Recently, researchers found that a new nanoparticle that combines chemotherapy and photodynamic therapy may enhance the effects of immune checkpoint inhibitors, overcoming this problem.
The study, “Core-shell nanoscale coordination polymers combine chemotherapy and photodynamic therapy to potentiate checkpoint blockade cancer immunotherapy“, published in Nature Communications, shows that these nanoparticles can activate immune cells to attack hidden metastasis, with the potential to broaden the use of immunotherapy in patients with metastatic colon cancer.
“Everybody out there working in the cancer space is trying to figure out ways to enhance checkpoint blockade immunotherapy,” Wenbin Lin, James Franck professor in chemistry at University of Chicago and one of the scientists who conceived the new therapy, said in a press release. “In this work, we were able to achieve that.”
Although the survival rates for patients with localized colorectal cancer are high, they drop to about 12 percent in those whose cancers have spread to the liver, lungs, or peritoneum. Effective treatments are needed that not only eradicate primary tumors, but also metastatic tumors.
Immune checkpoint inhibitors, which target suppressive pathways in T-cells to strengthen their anti-tumor responses, have led to significant clinical advances and provided a new strategy to combat cancer. With the exception of metastatic melanoma, however, these therapies fail to generate durable responses.
Researchers believe that this happens because if a tumor has been growing for years, its immunogenicity is low (the ability of a tumor to recruit and be recognized by immune cells), meaning there are no T-cells to be activated by the checkpoint inhibitors.
“So what we’re trying to do is to come up with ways to recruit T-cells to the tumor,” said Lin. “And if you have a way to make the T-cells recognize cancer cells, the T-cell will be able to go in there and kill the cancer cells.”
The researchers hypothesized that combining a PD-L1 inhibitor with nanoparticles, which not only induce tumor cell death but also increase tumor immunogenicity, could improve the response to checkpoint blockade therapy and broaden the use of immunotherapy in metastatic colon cancer.
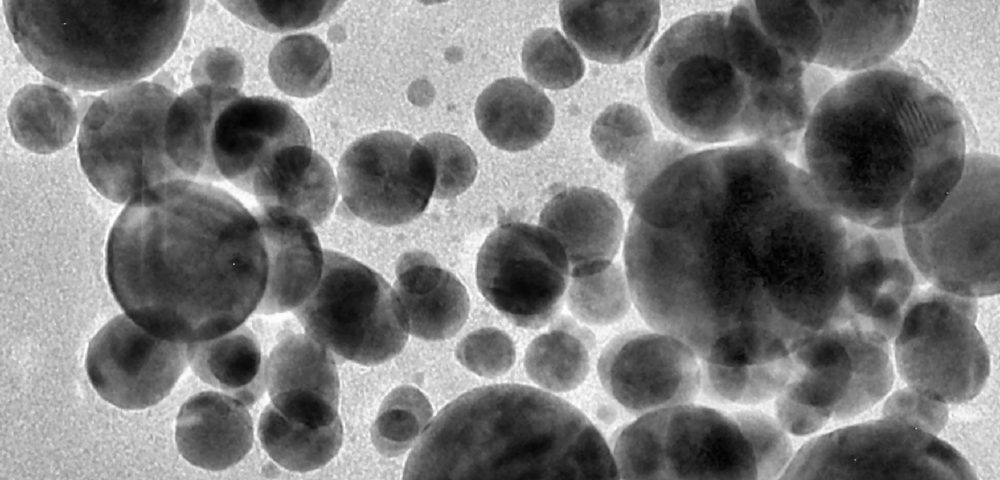
They developed nanoparticles that assemble themselves from zinc and Eloxatin (oxaliplatin), a U.S. Food and Drug Administration-approved chemotherapy for the treatment of colorectal cancer. The outer layer of these nanoparticles was composed of a photosensitive agent called pyrolipid, which generates reactive oxygen species that kill the cancer cells when exposed to light.
Researchers found that the nanoparticles had the ability not only to kill the cancer cells through the Eloxatin and toxic oxygen, but also to induce the expression of a protein that is widely recognized by immune cells, increasing tumor immunogenicity.
Importantly, when the nanoparticles and a checkpoint inhibitor were used in concert, even tumors that had not been treated and were distant from the treated tumor site were eliminated. In fact, when the researchers gave the two agents to mice with two tumors growing in different regions of the body and exposed one tumor to light to activate the pyrolipid, both tumors disappeared.
This was a surprise, since without light T-cells would not be active in the second tumor, “so we should not expect that tumor to disappear,” Lin said. “But we believe that this combination is able to activate the immune system to generate the T-cells that will recognize the cancer cells. Then they go around the body and kill the cancer cells in the distant site that has not been irradiated with the light.”
This effect, called abscopal effect, is a rare event that sometimes occurs in patients receiving radiation therapy, referring to the regression of tumors outside of the irradiated area. Although the mechanism is unknown, this study supports previous beliefs that the immune system plays a critical role.
The findings also point to the possibility of using these nanoparticles to fight metastasis often missed by clinicians.
“You cannot treat them because you don’t know where to look for them,” Lin said. “If you activate immune cells, they can home in to cancer cells selectively. So you have a better chance of getting rid of these small metastatic tumors throughout the body.”
Lin and colleagues have started a company to further develop this new therapy, and have raised initial funding to possibly take the therapy into clinical trials.