Researchers have uncovered an additional way through which colorectal cancer cells may acquire resistance to treatment. According to a recent study, published in Oncotarget, the cells that compose the tumor microenvironment can produce certain molecules that protect the tumor cells from the action of conventional chemotherapy.
The study, “Carcinoma-associated fibroblasts affect sensitivity to oxaliplatin and 5FU in colorectal cancer cells,” provides novel insights on the mechanisms through which cancer cells become resistance to certain treatments, which is one of the main obstacles that cancer patients face during the course of their diseases.
“Although current cancer research mainly focuses on therapies against specific targets, most tumors are still treated with conventional cytotoxic therapies, so drug resistance remains the main obstacle to their success,” David G. Molleví, PhD researcher of the Program Against Cancer Therapeutic Resistance (PROCURE) of IDIBELL (Bellvitge Biomedical Research Institute in Barcelona), said in a press release.
The study builds on the evidence that the tumor microenvironment is an important contributor to cancer progression. Researchers already knew that the cells within the tumor microenvironment (TEM) could be modified by the cancer cells to help them proliferate, but now there is increasing evidence that the TEM cells also can help cancer cells acquire resistance to therapies.
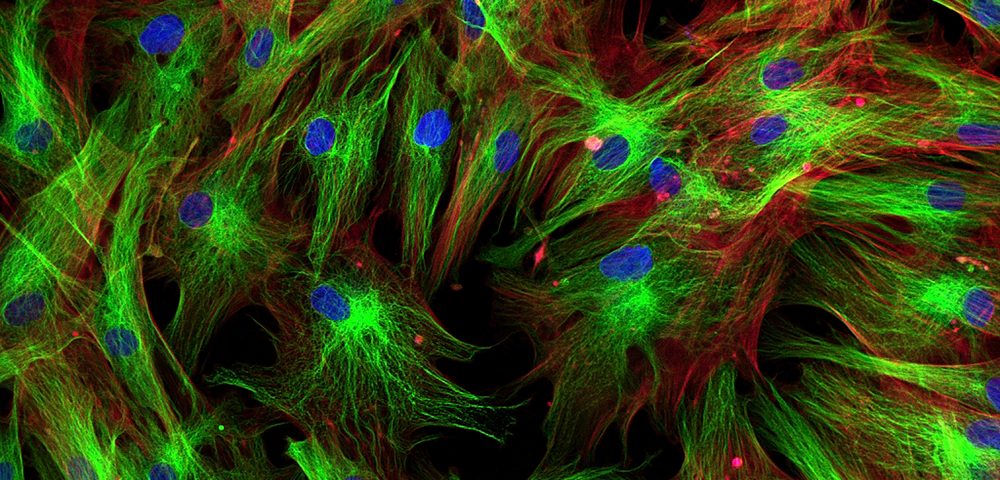
Researchers studied cancer-associated fibroblasts (CAFs), a component of the tumor microenvironment, and examined the soluble factors expressed by these cells. Certain molecules expressed by CAFs already had been linked with tumor aggressiveness and poor response to therapy, but how they affected colon cancer cells was poorly understood.
The investigators found that certain soluble factors trigger the activation of a cell-signaling cascade within the tumor cells that protected cells from the action of conventional chemotherapy used in colorectal cancer treatment. Specifically, the secreted molecules activated particular proteins in the cancer cells that ensured the correct DNA repair and cell cycle entrance, and thereby avoided the damage induced by the chemotherapeutic agents.
One of the pathways activated in the process was the JAK/STAT signaling pathway, causing researchers to believe that combining JAK/STAT inhibitors with conventional chemotherapy agents for colorectal cancer may improve treatment effectiveness and patients’ outcomes.
“From a clinical perspective, identifying the soluble factors that mediate such microenvironment-mediated drug resistance might yield valuable information to circumvent it,” said Molleví, lead author of the study. “Hampering key common, normal cells responsible for the synthesis of such factors might be an interesting approach to avoid the protective effect exerted by such molecules and to render tumor cells sensitive to chemotherapy,” he said.