Researchers at the University of Pittsburgh found that radiofrequency ablation (RFA) combined with an immune checkpoint inhibitor resulted in a stronger antitumor immunity with extended survival in human samples of primary colon tumor with liver metastasis and mice models of the disease.
The findings, titled “PD-1 Blockade Boosts Radiofrequency Ablation–Elicited Adaptive Immune Responses against Tumor,“ were published in Clinical Cancer Research , a journal of the American Association for Cancer Research.
Colorectal cancer is a disease causing abnormal growth of cells found in the lining of the colon or rectum, largely as a result of genetic mutations. The spread of the tumor cells to other parts of the body, mostly to the liver, is called metastasis of colorectal cancer.
“Liver is the most common site of colorectal cancer metastasis, and about 20 percent of colorectal cancer patients have liver metastases at the time of diagnosis [synchronous liver metastases],” Binfeng Lu, Ph.D., an associate professor in the Department of Immunology at the University of Pittsburgh, said in a press release.
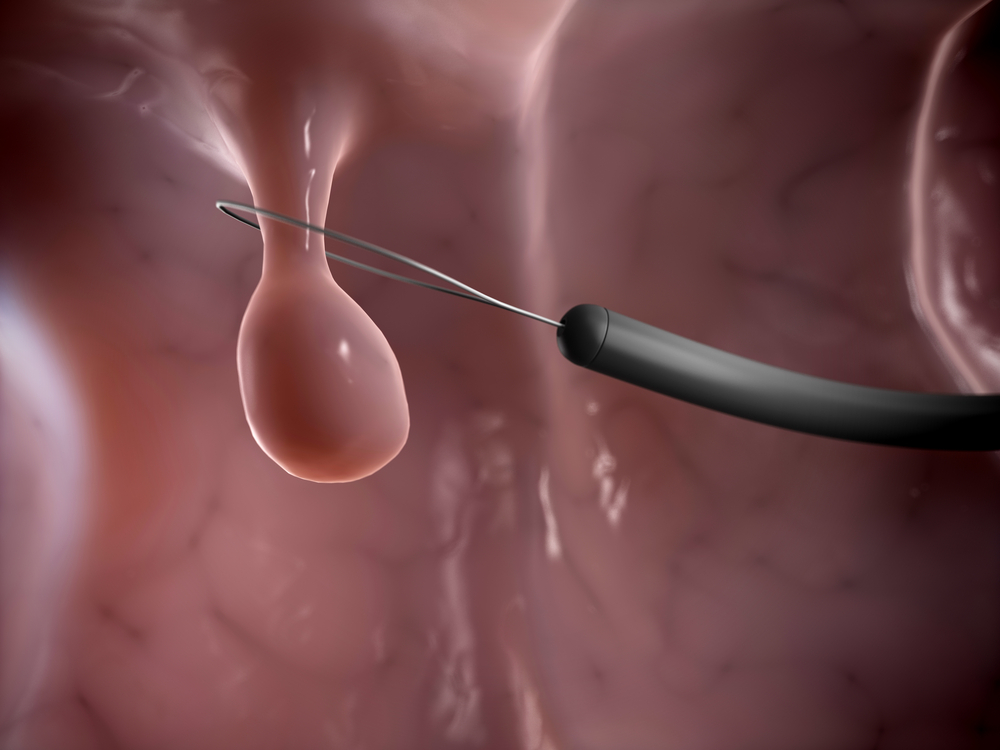
After colorectal cancer patients are diagnosed with liver metastasis, the best alternative treatment to surgery is RFA, especially for patients with smaller size liver nodules. The procedure uses imaging guidance to position a needle electrode through the skin into the liver tumor, where medium frequency alternating currents (350–500 kHz) pass through the electrode to induce heat that destroys tumor cells. However, RFA has little effect in stopping cancer from progressing, so researchers have investigated the immune-suppressive mechanisms limiting the efficiency of RFA.
“RFA is mainly recommended as local treatment for its physical effect of tumor destruction presently, and its immune effect has not been well studied. Our study revealed that RFA elicits systemic antitumor responses, and combining this with immune checkpoint blockade can potentially unleash the powerful immunotherapeutic effect of RFA,” Lu said.
A total of 78 samples taken from patients suffering from colorectal tumors with liver metastases were examined, of which 38 were treated with RFA for liver metastases before treatment of the primary colorectal tumors. The researchers found that RFA increased the number of immune white cells (T-cells) as well as the expression of an immune-inhibitory protein called PD-L1 at the location of the primary colon tumor. In mouse models, administration of an anti-PD-1 antibody inhibited RFA induced PD-L1.
“These studies show that liver RFA results in systematic inflammatory responses in the primary colon tumors and makes them more accessible to T-cells. These properties of RFA suggest it can potentially be used to make colorectal cancer patients who are nonresponsive to PD-1-based immunotherapy become responsive,” Lu said.
Moreover, combined treatment of both RFA and PD-1 was more efficient than separate treatments of RFA or PD-1 alone.
“These studies suggest that RFA complements and synergizes with anti-PD-1 immunotherapy,” Lu said. “As immune checkpoint inhibitors become available to colorectal cancer patients in the clinic, RFA might be used as adjuvant immunotherapy in patients with multiple metastases.”
The researchers intend to start a Phase 1 clinical study to investigate the efficacy of a combined therapy based on both RFA and anti-PD-1 antibody in patients with colorectal cancer and liver metastases.