Researchers at the University of California, San Diego School of Medicine made a surprising discovery that is published ahead of print in the prestigious journal Cell.
Researchers at the University of California, San Diego School of Medicine made a surprising discovery that is published ahead of print in the prestigious journal Cell.
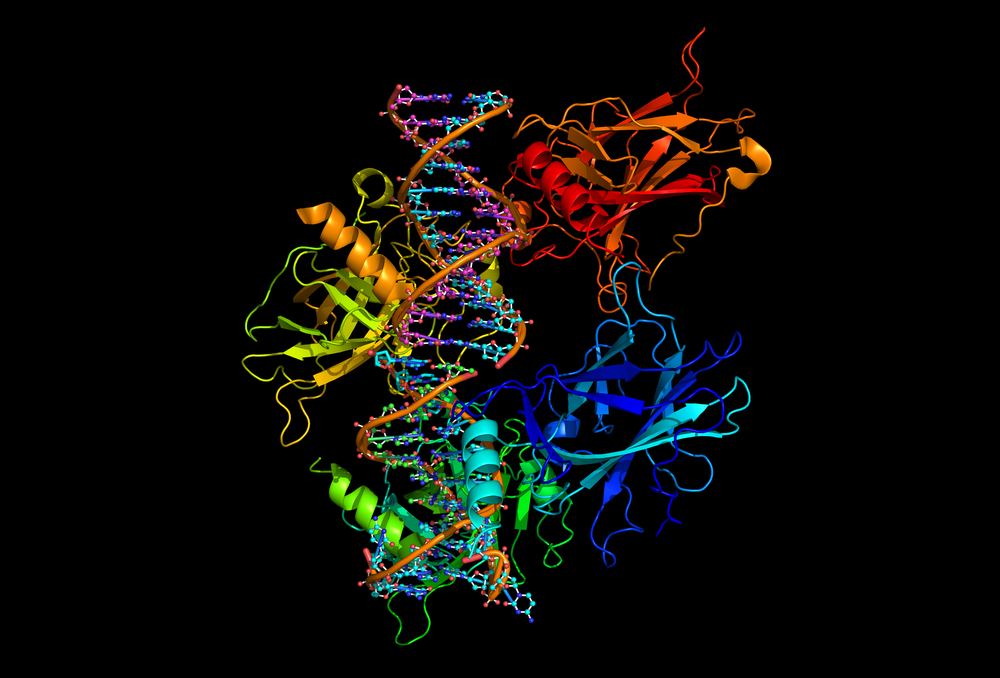
The team found that a set of specific enzymes (which are highly selective catalysts helping complex chemical reactions) actually suppress colon tumors instead of promoting their development, as had been postulated thus far. This specific set of enzymes is called Protein Kinase C (PKC).
PKC was thought to be involved in cancer-relevant activities, like cell survival, proliferation, migration and apoptosis. Efforts have been made from a clinical point of view to develop inhibitor-based drugs for PKC.
“For three decades, researchers have sought to find new cancer therapies based on the idea that inhibiting or blocking PKC signals would hinder or halt tumor development,” explained the study’s principal investigator Dr. Alexandra Newton in a news release, “but PKCs have remained an elusive chemotherapeutic target.” The authors suggest this is due to the fact that PKCs, instead of promoting cancer development as believed, in fact block tumor growth.
The team recurred to live cell imaging to analyze around 8 percent of more than 550 mutations present in PKC found in human cancers. Of all the mutations analyzed, none activated PKC, in fact, the majority reduced or abolished PKC’s activity since they were present in regions that blocked signal binding, prevented its correct structuring or affected the catalytic activity of the enzyme.
Using a colon cancer cell line, the researchers corrected one of the many loss-of-function mutations in PKC. Using a mouse model, they found that such correction resulted in a reduction of tumor growth, suggesting that a normal functional PKC activity does inhibit cancer development. The authors propose that in normal conditions, PKC would repress signaling of oncogenes (genes that have the potential to induce normal cells to become cancerous). Once PKC is not functional, oncogenic signaling is no longer repressed, resulting in an induction of cancer development.
“Inhibiting PKC has so far proved not only an unsuccessful strategy in a number of cancer clinical trials, but its addition to chemotherapy has resulted in decreased response rates in patients,” said Dr. Newton. “Given our results, this isn’t surprising. Our findings suggest therapeutic strategies need to go the other way and target ways to restore PKC activity, not inhibit it. This is contrary to the current dogma.”
This misinterpretation concerning the role of PKC in cancer may have occurred due to the fact that PKCs are receptors for tumor-producing phorbol esters, and, according to Dr. Corina Antal, the study’s first author, long-term activation of PKCs by phorbol esters results in their degradation. In current mouse models used to study tumor promotion, a carcinogen is applied on the animal skin followed by several phorbol esters’ applications. “This repeated application of phorbol esters will lead to the loss of PKC. Thus, their tumor-promoting function may arise because a brake to oncogenic signaling has been removed”, explained Dr. Antal. This observation may explain how researchers got mislead on the real function of PKCs in cancer.