 An “excellent” study–defined as such by meeting the randomized controlled trial requirement of Level I Evidence in medicine–from the Fox Chase Cancer Center and Jefferson Medical College in Pennsylvania and the Cancer Institute of New Jersey suggests that patients do not alter their preventative action behaviors against colorectal cancer in response to genetic and environmental risk assessment (GERA). Patients with an elevated risk for colorectal cancer found by GERA were just as likely to be screened for colorectal cancer as those with a moderate or low risk for colorectal cancer.
An “excellent” study–defined as such by meeting the randomized controlled trial requirement of Level I Evidence in medicine–from the Fox Chase Cancer Center and Jefferson Medical College in Pennsylvania and the Cancer Institute of New Jersey suggests that patients do not alter their preventative action behaviors against colorectal cancer in response to genetic and environmental risk assessment (GERA). Patients with an elevated risk for colorectal cancer found by GERA were just as likely to be screened for colorectal cancer as those with a moderate or low risk for colorectal cancer.
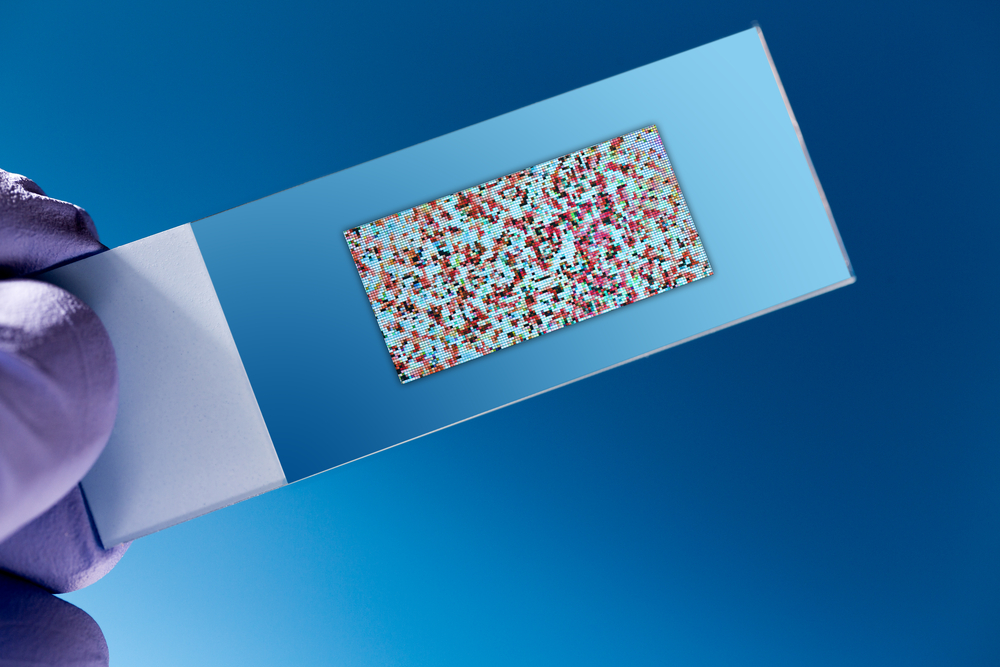
The gene of interest used by the researchers, as described in “Genetic and Environmental Risk Assessment and Colorectal Cancer Screening in an Average-Risk Population: A Randomized Trial,” was MTHFR, which encodes for methylenetetrahydrofolate reductase and regulates cellular folate metabolism, as folate receptors are highly expressed by certain types of cancer cells. Although the researchers noted that cancer usually arises from multiple mutations, which could also include those in the adenomatous polyposis gene (APC) in the case of colorectal cancer, they focused on MTHFR polymorphisms due to an association between serum folate levels and colorectal cancer risk.
Each patient enrolled in the experimental group was assessed for mutations in MTHFR (the genetic risk component) and serum folate (the environmental risk component) and then questioned about behaviors after three weeks and six months.
After six months, the rate of colorectal cancer screening was similar between the group receiving GERA and another group who did not receive GERA. The research seems to suggest that if an individual is at risk for colorectal cancer due to the presence of a moderately-associated risk factor (MTHFR mutations) instead of a highly-associated (90% association) risk factor (APC), he or she is no more likely to seek screening for colorectal cancer. While a handful of the 509 experimental participants who completed the study had an increase in distress following GERA, the feeling did not seem to alter screening rates.
Although the study shows no association between GERA risk in an average-risk population, this does not mean individuals did not change their behaviors following risk assessment. Colorectal cancer screening was the only metric used. It is unknown if participants chose to engage in other risk reduction strategies such as maintaining a healthy weight, achieving appropriate nutrient intake, and exercising.